
Dr Colum Nolan
Senior Consultant Spine & Neurosurgeon
MB, BCh, BAO, LRCPSI, MRCSI, FRCSI (Neurosurgery)
Spinal infections are rare but can be life-threatening. They can be caused by a bacterial or fungal infection elsewhere in the body, carried to the spine through the bloodstream. Staphylococcus aureus and Escherichia coli are two bacterium that are the most common sources of spinal infections.
Spinal infections can also occur up to 3 months post-operation. For example, patients who have undergone a urological procedure may be prone to spinal infections because the veins in the lower spine come up through the pelvis. Patients undergoing dental procedures are also at an increased risk of spinal infections, because bacteria may be introduced into the bloodstream during the procedure.

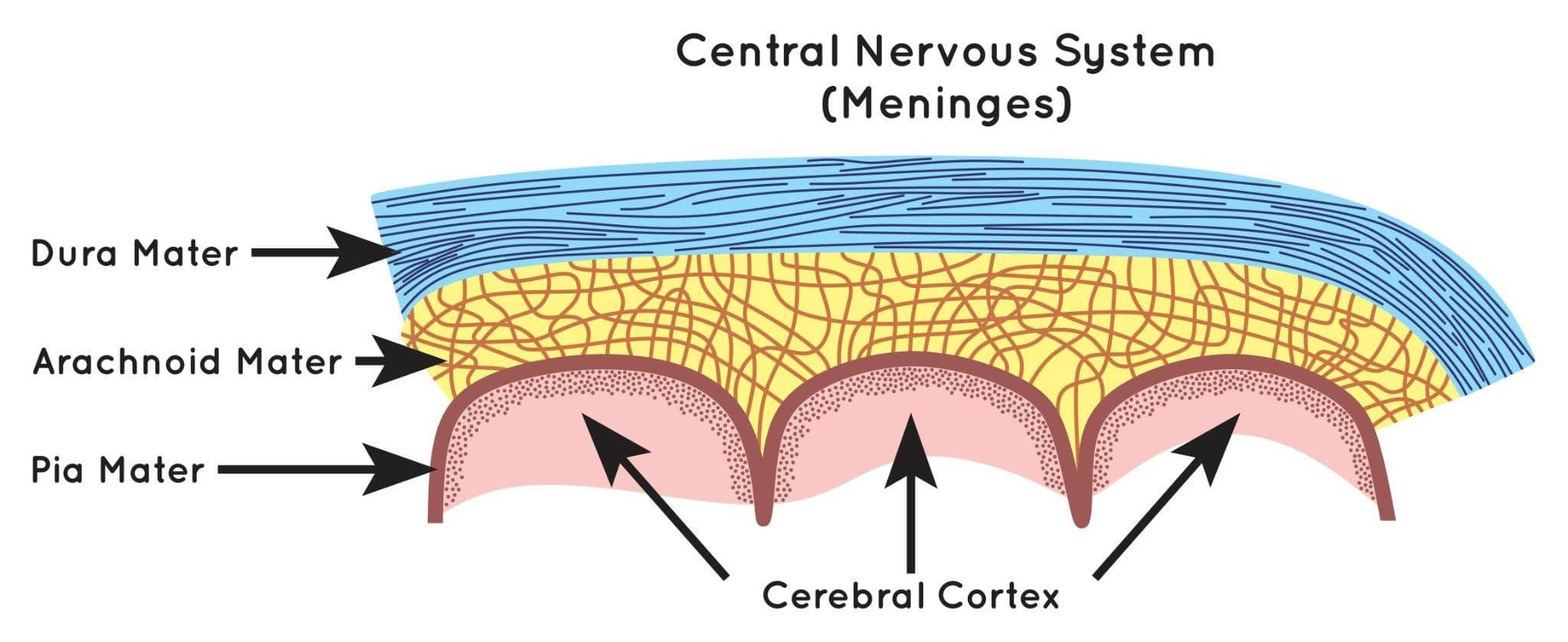
Spinal infections can be broadly classified according to the location they occur in. Different types of spinal infections present with different symptoms.
The main telltale sign of osteomyelitis is pain in the spine – one that worsens at night and persists over time. Other symptoms include;
Spinal infections are uncommon but certain factors increase our risk of developing one. Age, for one, is associated with spinal infections because as we get older, our immune system becomes weaker and less able to defend against infections.
Other medical conditions that compromise the immune system include HIV infections, diabetes mellitus, cancer, and malnutrition. Persons who are on long-term systemic usage of steroids or intravenous drug use are also more susceptible to spinal infections.
Spinal infections can also develop as a result of surgery, especially surgeries of long duration, and involve high blood loss, organ transplantation, and implantation of instruments.
Oftentimes, the main symptom of a spinal infection is pain, which is not an uncommon symptom of other conditions. This makes spinal infections more challenging to diagnose early, because many patients do not seek medical attention until more progressive symptoms appear.
Spinal infections are typically diagnosed using a combination of laboratory and imaging tests.
Special laboratory tests can determine the presence of an infection by monitoring for inflammation within the body. If there is an infection present, the next step is to identify the cause of infection. This can be done through biopsy of the vertebrae or disc space, or blood cultures.
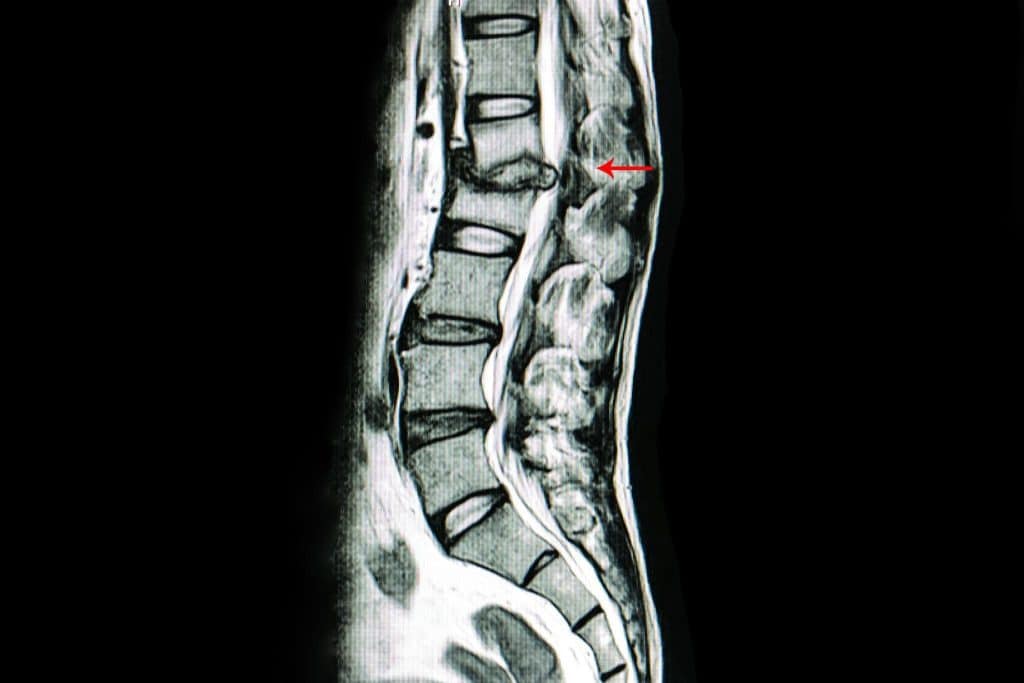
An MRI scan can produce the most accurate, detailed images of the spine including the spinal nerves, spinal cord, paraspinal muscles, and adjacent soft tissues around the spinal column. However, it is only ordered after other pathologies, such as inflammation or tumours, are ruled out.
Spinal infections can deal irreversible damage to your spine and the areas around it, if left untreated. If you suspect you have a spinal infection, please consult a neurosurgeon immediately and get a proper diagnosis.

As a first course of defence, after identifying the organism causing the infection, Dr Nolan will prescribe antibiotics to treat the spinal infection. The course of antibiotic or antifungal therapy is long-term and can mean extended hospitalisation for the patient. Other non-surgical options, such as a back brace or bed rest, may be recommended where surgery is not required.
However, if the spinal infection has resulted in spinal instability or you have started developing neurological symptoms, surgery is highly recommended. The primary goals of surgery are to remove the infected tissue and restore spinal stability. This process would also help to restore any loss in neurological function.
Dr Colum Nolan is a Senior Consultant Neurosurgeon with over 20 years of experience, specialising in minimally invasive spine (keyhole) surgery and other spine procedures.
A graduate of the Royal College of Surgeons in Ireland, Dr Nolan underwent neurosurgical training in Ireland and Australia, followed by a fellowship in complex spine surgery at Addenbrooke’s Hospital, Cambridge, as well as rotations at the Orthopaedic Spine Unit in Norfolk and Norwich Hospital.
Dr Colum is committed to delivering compassionate, patient-centred care, combining surgical precision with a genuine dedication to improving his patients’ quality of life.

Make an Enquiry or Request an Appointment
Our friendly team is here to serve you. For urgent enquiries and appointment requests, please call or WhatsApp us directly.