Low back pain is a common symptom most patients express to health practitioners. As reported by the Ministry of Health Singapore’s HealthHub, up to 80% of Singaporeans suffer from low back pain in their lifetime. With a myriad of causes, low back pain can be caused by age-related spine changes, spinal stenosis (narrowing of the spinal canal), herniated discs (bulging spinal discs pressing on nearby nerves.), bad posture, and fibromyalgia (a condition causing widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive difficulties), among others.
Exercise, physical therapy, and over-the-counter medications are non-surgical approaches to managing back pain. However, suppose non-surgical techniques fail to achieve the desired symptom relief, and you still have severe and persistent lower back pain caused by a bulging disc. In that case, your neurosurgeon may counsel you to undergo a minimally invasive lumbar discectomy and decompression.
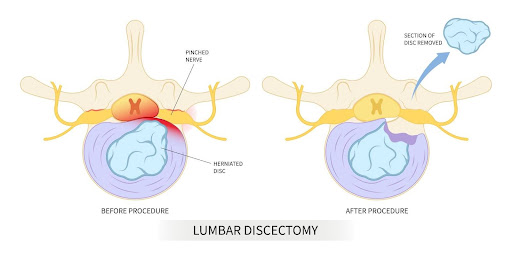
A minimally invasive lumbar discectomy and decompression (also called microdiscectomy of the lower back) is a type of Minimally Invasive Spinal Surgery (MISS) which relieves symptoms of a compressed nerve by removing all or part of a herniated disc. A small 1 to 2-inch incision will be made in your back at the level of the affected disc. Through the incision, a small tube is inserted into your back. Through the tube, a scope (a small camera used to view internal structures), a light source and a small tool are inserted to remove the affected disc. The affected vertebrae may be fused together following the disc removal.
Minimally invasive lumbar discectomy and decompression uses small incisions and a scope which is different from the older and more traditional open lumbar discectomy, where larger incisions are made in the back, which usually results in more pain, more muscle and tissue loss, and a longer recovery time.
At Oxford Spine and Neurosurgery Centre, a specialist clinic in Singapore, our Senior Consultant Neurosurgeon has particular expertise in minimally invasive spine surgery. He has successfully completed many minimally invasive lumbar discectomy and decompression surgeries, helping patients to enjoy relief from their symptoms.

The lower spine is made up of five bones which are identified as L1, L2, L3, L4 and L5. The vertebral, spine or spinal column extends from the neck to the tailbone. It comprises thirty-three (33) vertebrae divided into seven cervical bones in the neck region; twelve thoracic bones in the chest region; five lumbar bones, five sacral bones and four coccygeal bones that make up the tailbone. These bones provide passage for the spinal cord and the spinal nerves. Intervertebral discs sit between vertebrae and prevent excessive wear and tear from friction, offer protection, and act as both a cushion and a shock absorber.
Intervertebral discs can sometimes bulge, slip, or herniate, exerting pressure on adjacent nerves. Herniated discs are more common in the lumbar vertebrae, and the L4-L5 and L5-S1 vertebrae are most affected.

Your neurosurgeon will determine if you need a surgical or non-surgical treatment for your individual condition. Your neurosurgeon will take into consideration:
At Oxford Spine and Neurosurgery Centre, Dr Colum Nolan, our experienced neurosurgeon in Singapore, will thoroughly assess your condition and recommend a tailored treatment plan. For instance, he will let you know whether minimally invasive lumbar discectomy and decompression are suitable for you.
A minimally invasive lumbar discectomy and decompression’s greatest benefit is the relief it offers from your back pain. Other benefits are:

Preparation for a minimally invasive lumbar discectomy and decompression may involve the following:
During a minimally invasive lumbar discectomy and decompression surgery, you will first be administered anaesthesia. You will then be connected to machines to monitor your vital signs, such as your blood pressure, heart rate, oxygen saturation, and respiratory rate. You will be placed in a prone or face-down position on the operating table.
Once the anaesthesia takes effect, your surgeon will begin the procedure. Your doctor will make a small 1 to 2-inch incision in your back at the level of the affected disc. Particular types of X-rays are also used to determine the vertebrae and intervertebral discs affected. A small tube is inserted into your back through the incision made. A scope ( a small camera used to view internal structures), a light source and a small tool are inserted to remove the affected disc through this tube. This may be followed by fusing the vertebrae involved. After the affected disc is removed, the incision is sutured or stapled.
Following your procedure, your vital signs will still be monitored, and you will be sent to the recovery ward for observation for some hours since the surgery can be done as an outpatient procedure or a day case. Pain and discomfort may be felt following the procedure, and you will be given pain medications.
You will receive instructions on limiting heavy lifting, strenuous exercises, and bending. Your neurosurgeon may also recommend physical therapy, and you may need to wear a back brace during your immediate recovery period. You will be given follow-up appointments, and it is important to attend your appointments for continued care and monitoring.
A minimally invasive lumbar discectomy and decompression has a success rate of 80% – 90% in relieving symptoms in patients. In a 25-year retrospective study of 201 patients who underwent the procedure, a 90% success rate was recorded.
Common risks or side effects associated with a minimally invasive lumbar discectomy and decompression include:
Rest assured that a skilled neurosurgeon will be able to lower the risk of experiencing post-surgical side effects,
The recovery time for a minimally invasive lumbar discectomy and decompression is shorter and better than that for an open lumbar discectomy. Immediate recovery time is several weeks, and it will largely vary per individual depending on your health status, the complexity of your surgery, and the presence or absence of complications.
You may experience pain in the first few weeks following your procedure, and adherence to your prescribed pain medications is recommended.
For personalised guidance on your suitability for minimally invasive lumbar discectomy and decompression, please book an appointment with Oxford Spine and Neurosurgery Centre to consult Senior Consultant Neurosurgeon Dr Colum Nolan.
Dr Colum Nolan is the Medical Director at Oxford Spine and Neurosurgery Centre, Mount Elizabeth Novena Hospital in Singapore. He is an experienced Senior Consultant Neurosurgeon with a subspecialty in Spine Surgery.
With over 15 years of experience, Dr Colum’s clinical interests include degenerative and complex spinal disorders, cervical spine surgery, spinal tumours, spinal trauma, and endoscopy. He has particular expertise in minimally invasive spine surgery and spinal navigation technology for enhanced accuracy and safer surgery, and he uses techniques such as artificial cervical disc replacement as an alternative to spinal fusion.
