
Dr Colum Nolan
Senior Consultant Spine & Neurosurgeon
MB, BCh, BAO, LRCPSI, MRCSI, FRCSI (Neurosurgery)
Lumbar spinal stenosis is characterised by the narrowing of the lumbar spinal canal (the space around the spinal nerves) and compression of the nerves that travel through the spine and into the legs. This causes pain to radiate downwards to your feet as you walk. It may also cause weakness or numbness when you walk. Spinal stenosis can occur in any part of the spine, but it is more common in the lower back (lumbar region).
It is a condition that occurs gradually over the years and hence, is often found to affect the middle-aged and elderly.
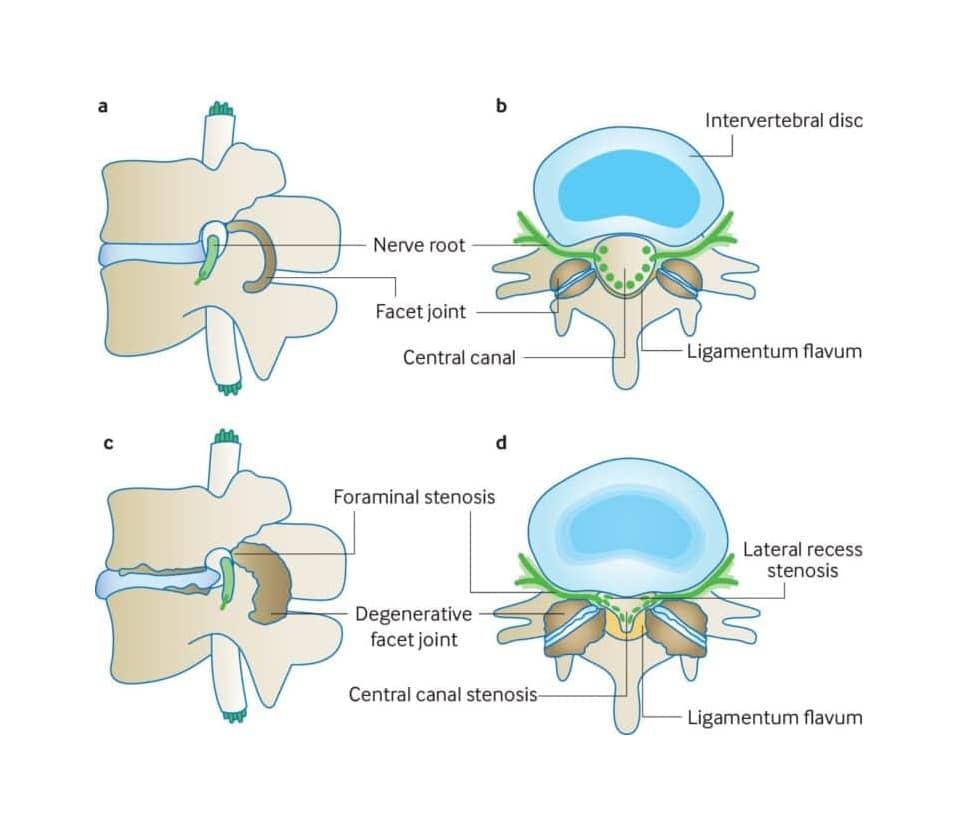
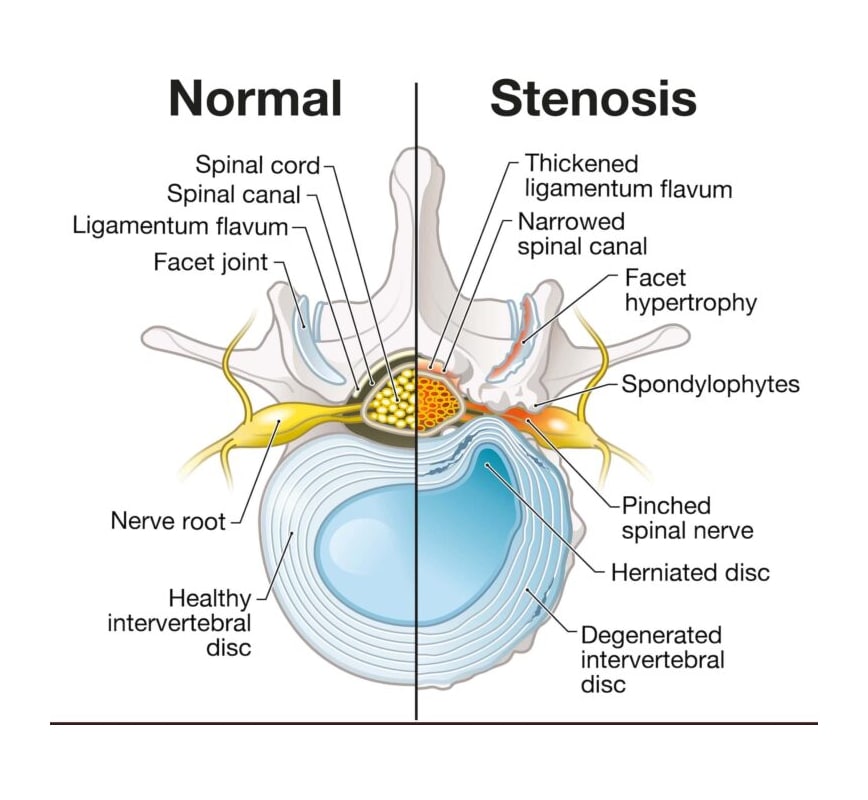
The lumbar spine is made up of five vertebrae (bones) along with accompanying intervertebral discs (‘cushions’ or ‘shock absorbers’) between the vertebrae. The discs consist of a soft jelly-like centre (nucleus) contained by a thick, tougher exterior (annulus). The joints between the bones are called facet joints and are lined with cartilage. Ligaments also connect the bones to each other. These structures allow the movement of the back and control stability and flexibility.
Lumbar spinal stenosis is found to be a result of many age-related changes such as
As we grow older, our spinal discs often degenerate, thin out, and bulge. These changes can narrow the spinal canal and contribute to stenosis. Small tears may form in the lining of the disc, allowing the soft centre to push outwards and press on the nerves.
A herniated or slipped disc occurs when a tear in the outer lining of the disc allows part of the soft centre to protrude more prominently into the spinal canal. This can press on the nerves and contribute to stenosis.
The ligaments between the bones can stiffen over time and may thicken or buckle into the spinal canal. When this occurs, they take up additional space around the nerves and add to the narrowing.
As part of the degenerative process, changes can also occur in the facet joints. These joints may become enlarged through overgrowth (hypertrophy), and fluid collections (effusions) can develop. In some cases, facet joint changes, together with disc and ligament degeneration, can lead to instability in the spine. This instability may cause one vertebra to slip forward relative to another, a condition known as spondylolisthesis, which can further worsen the stenosis.
The spine’s misguided effort to strengthen itself can cause tiny bone growths or bone spurs to form in response to natural wear-and-tear from osteoarthritis. These bone spurs can project into the spinal canal and compress the nerves.
Although uncommon, tumours in or around the spine can take up space within the spinal canal and lead to nerve compression.
Risk factors increase the likelihood of developing stenosis but do not directly cause the anatomical narrowing. These factors make someone more prone to the degenerative changes described above.
With spinal stenosis, one common symptom is pain in the legs or calves and lower back after walking. This pain is eased when sitting down or leaning over because more room is created for the spinal canal in these postures.
Not all patients will develop symptoms. It remains unknown why some patients are more susceptible to developing symptoms, while others are not.
The risk of spinal stenosis is greater in females aged 50 and older. Those born with a narrow spinal canal or have had previous injury to the spine are also more likely to suffer from this condition.
Although spinal stenosis is usually clinically diagnosed based on history taking and physical examination, the symptoms can mimic other conditions so a proper assessment is important. Imaging studies such as X-rays and MRI scans are typically used to investigate further. An MRI, in particular, would be useful to determine the nature and extent of the spinal stenosis. X-rays show the bony outline and the alignment of the bones in the back and MRI scan will be able to visualise the structures in your spine such as the discs, ligaments, joints, muscles and the spinal cord and the nerves. In some cases a CT scan is also done to assess the bony structures in more detail and to look at the extent of any bone spurs.
In the absence of progressive neurological symptoms, spinal stenosis can be managed initially through non-surgical methods such as physical therapy and medications (anti-inflammatory medications or painkillers). You may be encouraged to try selected aerobic activities such as swimming or stationary cycling. These endurance exercises help to maintain motion of the spine, while strengthening abdominal and back muscles.
In cases where your symptoms remain troublesome despite medication and physical therapy, steroid injections may be useful (epidural or nerve block) in an attempt to try to avoid the need for surgery.
Surgery would be considered for patients whose symptoms are severe despite other treatments and significantly affecting their lifestyle. Surgery may also be recommended if there is weakness or disturbance of bowel or bladder function. The purpose of surgery is to relieve pressure on the nerves by removing part of the hypertrophied bone and thickened ligament and/or bulging disc through a procedure referred to as lumbar decompressive laminotomy. This can typically be done via minimally invasive techniques, avoiding the need for open surgery.
In cases where there is significant instability of the spine, a spinal fusion may be necessary to stabilise the spine. This typically involves insertion of titanium screws into the affected vertebrae which are connected and secured with rods and insertion of a spacer and bone graft into the disc space to fuse the bones together. This can usually also be done using minimally invasive techniques.
If these symptoms sound familiar, it may be time to get a specialist assessment for possible lumbar spinal stenosis.
Book a consultation with Oxford Spine and Neurosurgery Centre to identify the cause early and receive guidance on suitable care options.
Although spinal stenosis is usually diagnosed through history taking and physical examination, its symptoms can resemble other conditions, so a proper assessment is essential. Imaging studies, such as X-rays and MRI scans, are commonly used to further investigate. An MRI is particularly valuable for determining the nature and extent of the stenosis, as it provides detailed views of the discs, ligaments, joints, muscles, spinal cord and nerves. X-rays show the bony outline and alignment of the spine, while a CT scan may be used in selected cases to assess the bony structures in greater detail and evaluate the presence of bone spurs.
In the absence of progressive neurological symptoms, lumbar spinal stenosis can often be managed first with non-surgical treatments. These may include physiotherapy and medications such as anti-inflammatory drugs or painkillers. You may also be encouraged to try selected aerobic activities, including swimming or stationary cycling. These endurance exercises help maintain spinal mobility while strengthening the abdominal and back muscles.
If symptoms continue to be troublesome despite medication and physiotherapy, steroid injections may be considered. Epidural injections or targeted nerve blocks can reduce inflammation around the nerves and may help avoid the need for surgery.
Surgery for lumbar spinal stenosis may be considered when symptoms remain severe despite conservative treatment, or when there is weakness or disturbance of bowel or bladder function. The goal of surgery is to relieve pressure on the nerves by widening the spinal canal or the openings where nerves exit the spine. Several techniques may be used, depending on the exact cause and location of the compression, and many of these procedures can be performed using minimally invasive methods.
Ready to explore a treatment plan that works for you?
Consult Dr Colum Nolan to review the evidence-supported options and understand what each might mean for your recovery.

Maintaining a healthy spine is an important part of reducing the likelihood of symptoms from lumbar spinal stenosis. Regular physical activity plays a key role, as movement helps keep the spine flexible and strengthens the muscles that support it. Activities such as walking, swimming, cycling, and light weight training are often recommended because they place less strain on the back while still building strength and endurance.
Alongside exercise, keeping your weight within a healthy range can lessen the load on the lower spine, which may slow age-related wear. Everyday habits also matter. Paying attention to posture and using proper bending and lifting techniques can help protect the spine during routine tasks and reduce the chance of irritation or injury.
Although these measures cannot fully prevent spinal stenosis, they can support overall spinal health and may lessen the impact of age-related changes over time.
Lumbar spinal stenosis occurs when the space around the spinal nerves in the lower back becomes narrowed, leading to nerve compression. This can cause pain in the legs or lower back that worsens with walking and improves when sitting or leaning forward. Some people also experience numbness, tingling, burning or a sense of weakness. In severe cases, bowel or bladder control may be affected.
Lumbar spinal stenosis usually develops due to age-related changes such as disc degeneration, thickened ligaments, facet joint enlargement or herniated discs. Bone spurs or conditions like spondylolisthesis can also contribute. Risk increases with ageing, arthritis, previous spinal injuries, congenital narrowing, scoliosis, obesity and long-term poor posture. These factors do not directly cause stenosis but make degenerative narrowing more likely over time.
Treatment depends on symptom severity. Most people start with physiotherapy, anti-inflammatory medication, pain relief and mobility exercises. If symptoms persist, steroid injections or nerve blocks may help reduce inflammation. Surgery is considered when pain remains severe despite conservative care or when weakness or bowel or bladder issues occur. Procedures aim to relieve pressure on the nerves and may be performed using minimally invasive techniques.
Although lumbar spinal stenosis cannot be fully prevented, healthy habits can reduce its impact. Regular exercise helps maintain flexibility and strengthen the muscles that support the lower back. Low-impact activities such as walking, swimming or cycling are often recommended. Keeping a healthy weight reduces strain on the spine, while good posture and proper lifting techniques help protect the back during daily activities.
Yes, lumbar spinal stenosis can return after surgery. Although many patients experience long-lasting relief, surgery does not stop age-related changes in the spine. Degeneration of discs, ligaments or joints may lead to renewed narrowing at the same level or a nearby one. Conditions such as spondylolisthesis can also contribute. If symptoms recur, treatment often starts with physiotherapy, medication or injections, with further surgery considered only when necessary.
Dr Colum Nolan is a Senior Consultant Neurosurgeon with over 20 years of experience, specialising in minimally invasive spine (keyhole) surgery and other spine procedures.
A graduate of the Royal College of Surgeons in Ireland, Dr Nolan underwent neurosurgical training in Ireland and Australia, followed by a fellowship in complex spine surgery at Addenbrooke’s Hospital, Cambridge, as well as rotations at the Orthopaedic Spine Unit in Norfolk and Norwich Hospital.
Dr Colum is committed to delivering compassionate, patient-centred care, combining surgical precision with a genuine dedication to improving his patients’ quality of life.

Make an Enquiry or Request an Appointment
Our friendly team is here to serve you. For urgent enquiries and appointment requests, please call or WhatsApp us directly.