‘Shooting Pain’ and Numbness in Arm

Dr Colum Nolan
Senior Consultant Spine & Neurosurgeon
MB, BCh, BAO, LRCPSI, MRCSI, FRCSI (Neurosurgery)
Cervical radiculopathy, often called a pinched nerve in the neck, is a condition in which a nerve root in the cervical spine (neck) becomes compressed or inflamed. This affects normal neurological function. The nerve roots supply the muscles that control movement in the shoulders, arms and hands, and they also carry sensory signals from the skin of the upper limbs.
When these nerve roots are irritated or damaged, pain or altered sensation can occur in the shoulder, arm or hand, depending on which root is involved.
People with cervical radiculopathy commonly report neck pain that travels into the shoulder and sometimes down the arm into the hand or fingers. Tingling and numbness are frequent symptoms, and muscle weakness may develop if the condition progresses.

A variety of conditions can place pressure on a nerve root in the neck and lead to cervical radiculopathy. Some causes are related to natural age-related changes in the spine, while others are less common structural or medical issues. Understanding these underlying factors can help guide appropriate assessment and treatment.
Degeneration of the spine occurs as part of the natural process of ageing. Degeneration related to cervical osteoarthritis and/or cervical degenerative disc disease can result in the growth of bony spurs, thickening of ligaments, or bulging spinal discs that can put pressure on the nerve roots.
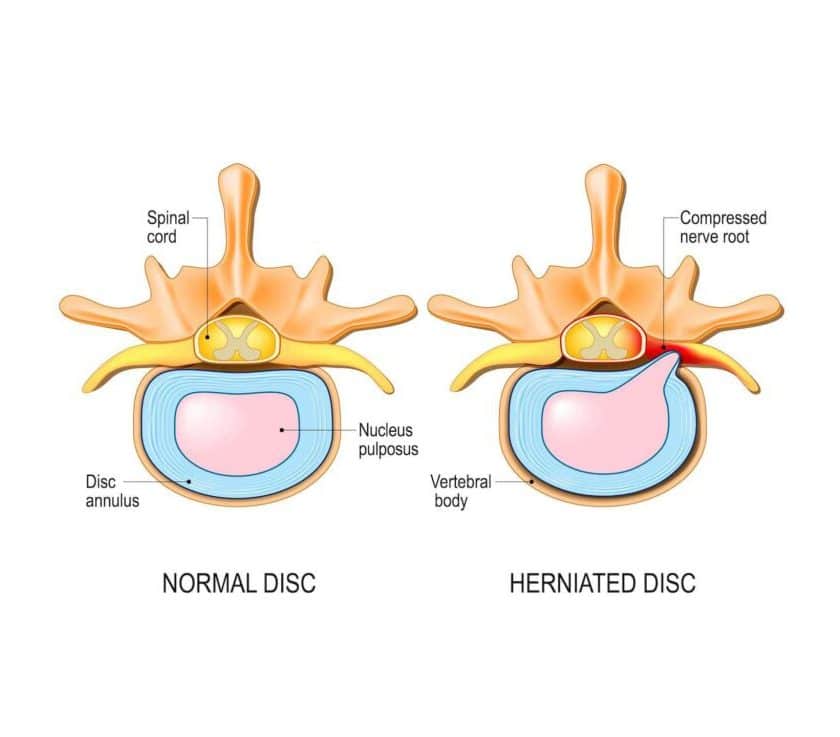
In younger people, pain, tingling sensations or numbness radiating down the arm may be the result of an injury that caused a ruptured or herniated spinal disc. Physical activities, such as heavy lifting or extreme sports, can cause a herniated spinal disc. When a spinal disc is herniated, the inner contents of the disc leak out and inflame the adjacent nerve.
A nerve root can also become compressed or impinged when the opening through which it exits the spinal canal narrows. This condition is also known as cervical foraminal stenosis. This narrowing of the opening can be the result of the conditions mentioned above.
Although rare, spinal infections can occur when a fungal or bacterial infection in another part of the body enters the spine through the bloodstream. Infected collections can irritate or compress nerve roots, causing cervical radiculopathy. TB infection can also occur in the spine.
Tumours arising in or near the spine can also irritate and compress the nerve roots in the cervical spine, resulting in symptoms suggestive of cervical radiculopathy.
All of these conditions may also cause compression of the spinal cord. When this occurs, it can lead to cervical myelopathy, a separate condition requiring prompt medical assessment.
Cervical radiculopathy can develop either suddenly or gradually, and symptoms may come and go.
The primary symptoms of cervical radiculopathy include pain that:
Changes in sensation are also common. Many people notice tingling, “pins and needles” or numbness that mirrors the pathway of the pain through the shoulder, arm and hand. These sensations may accompany pain or appear on their own. As the condition progresses, muscle weakness may develop in the shoulder, arm or hand.
The following additional symptoms may indicate that there is also cervical myelopathy due to spinal cord compression:

If any of these symptoms appear or worsen, it is best to make an appointment with our clinic for a thorough assessment and timely treatment.
The symptoms of cervical radiculopathy can develop suddenly or gradually and can be intermittent. The primary symptoms of cervical radiculopathy include pain that:
If you experience any of the following additional symptoms, it may indicate that there is also cervical myelopathy due to spinal cord compression:
Cervical radiculopathy can affect anyone, but some factors are known to increase the risk more than others.
Cervical radiculopathy occurs more often in males than females.
Cervical radiculopathy is more likely to occur in older persons as the spine degenerates as part of the ageing process. Some estimate that persons in the age group of 50 to 54 are at the highest risk of cervical radiculopathy. If it occurs in younger persons, it is more likely to be a result of an injury or herniated spinal disc.
Activities that place repeated or excessive strain on the neck can increase the risk. These include improper lifting techniques, heavy manual work or high-impact actions such as diving from a height.
A history of radiculopathy can make a person more susceptible to recurrence. It may also be associated with an increased risk of developing cervical myelopathy if further degenerative or structural changes occur.

To understand your pain better, you will be asked to describe your symptoms. This would include the location and extent of your pain and any activity or posture that possibly increases this pain. You should also share if you have experienced similar pain before, or if there was any recent injury.

A comprehensive physical examination will be performed by the cervical radiculopathy specialist to look for signs of cervical radiculopathy or cervical myelopathy. The examination will also be done to ensure there are no other problems that might be causing the symptoms like a local shoulder problem, for instance.

X-rays and MRI scans are typically used to investigate further. X-rays show the bony outline and the alignment of the bones in the neck, and an MRI scan will be able to visualise the structures in your spine, such as the discs, ligaments, joints, muscles, the spinal cord and nerves. In some cases a CT scan is also done to assess the bony structures in more detail and to look at the extent of any bone spurs.

In some patients, the symptoms of cervical radiculopathy improve on their own without specific medical intervention. When care is needed, treatment usually begins with non-surgical options. Conservative cervical radiculopathy treatment, also known as neck pain treatment, may include:
If symptoms remain severe despite these measures or persist for an extended period, further options may be considered. These can include a steroid nerve block to reduce inflammation around the affected nerve or, in selected cases, cervical radiculopathy surgery. A spine doctor in Singapore may recommend surgery if muscle weakness develops or if symptoms continue to interfere significantly with daily activities. The aim of surgery is to relieve pressure on the affected nerve and, when necessary, stabilise the spine.
Cervical radiculopathy occurs when a nerve in the neck is compressed or inflamed, which disrupts how signals travel to the shoulder, arm or hand. Persons may feel pain, tingling or weakness along the affected pathway. Age-related disc wear is the most common cause, although sudden disc herniation or trauma can also lead to symptoms.
This condition tends to arise when a disc, joint or surrounding tissue reduces the space available for a cervical nerve root. Disc degeneration, herniated discs and arthritic thickening are frequent culprits. Less often, acute injuries or repetitive strain place excess load on the neck. These changes can irritate the nerve and trigger pain or altered sensation.
Typical symptoms include neck pain that may travel into the shoulder, arm or hand. Some people notice tingling, numbness or a spreading pins and needles feeling. Weakness can occur when the nerve signal is more disrupted. Symptoms often vary with neck movement and may ease with simple rest or posture adjustments.
Yes, many cases resolve with conservative care. Rest, physiotherapy, posture guidance and suitable medication often lead to steady improvement over several weeks. Most people recover fully without surgery. Persistent or worsening symptoms, especially if accompanied by weakness, signal the need for medical review.
Surgery is considered when symptoms do not improve with non-operative treatment or when there is significant or progressive weakness. It may also be recommended if imaging shows clear nerve compression from a disc or bony change. The aim is to relieve pressure on the nerve, restore function and prevent lasting damage.
Dr Colum Nolan is a Senior Consultant Neurosurgeon with over 20 years of experience, specialising in minimally invasive spine (keyhole) surgery and other spine procedures.
A graduate of the Royal College of Surgeons in Ireland, Dr Nolan underwent neurosurgical training in Ireland and Australia, followed by a fellowship in complex spine surgery at Addenbrooke’s Hospital, Cambridge, as well as rotations at the Orthopaedic Spine Unit in Norfolk and Norwich Hospital.
Dr Colum is committed to delivering compassionate, patient-centred care, combining surgical precision with a genuine dedication to improving his patients’ quality of life.

Make an Enquiry or Request an Appointment
Our friendly team is here to serve you. For urgent enquiries and appointment requests, please call or WhatsApp us directly.