
Dr Colum Nolan
Senior Consultant Spine & Neurosurgeon
MB, BCh, BAO, LRCPSI, MRCSI, FRCSI (Neurosurgery)
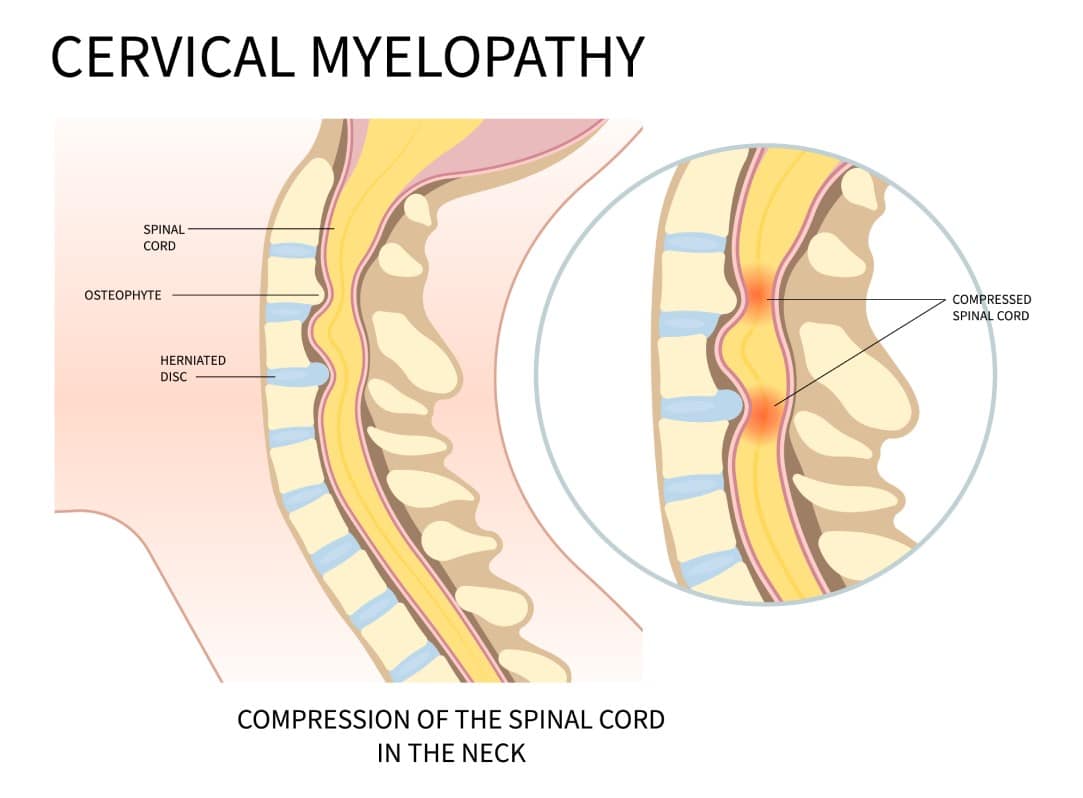
Cervical myelopathy is a degenerative condition that results from compression of the spinal cord in the neck. This compression could be a result of a traumatic impact or injury to the spine, degenerative disease, herniated discs or congenital narrowing of the spinal canal in the neck.
The cervical spine is made up of seven vertebrae (bones) along with accompanying intervertebral discs (‘cushions’ or ‘shock absorbers’) between the vertebrae. The joints between the bones are called facet joints and are lined with cartilage. Ligaments also connect the bones to each other. These structures allow the movement of the neck and control stability and flexibility.
Cervical myelopathy can occur due to several reasons, including:
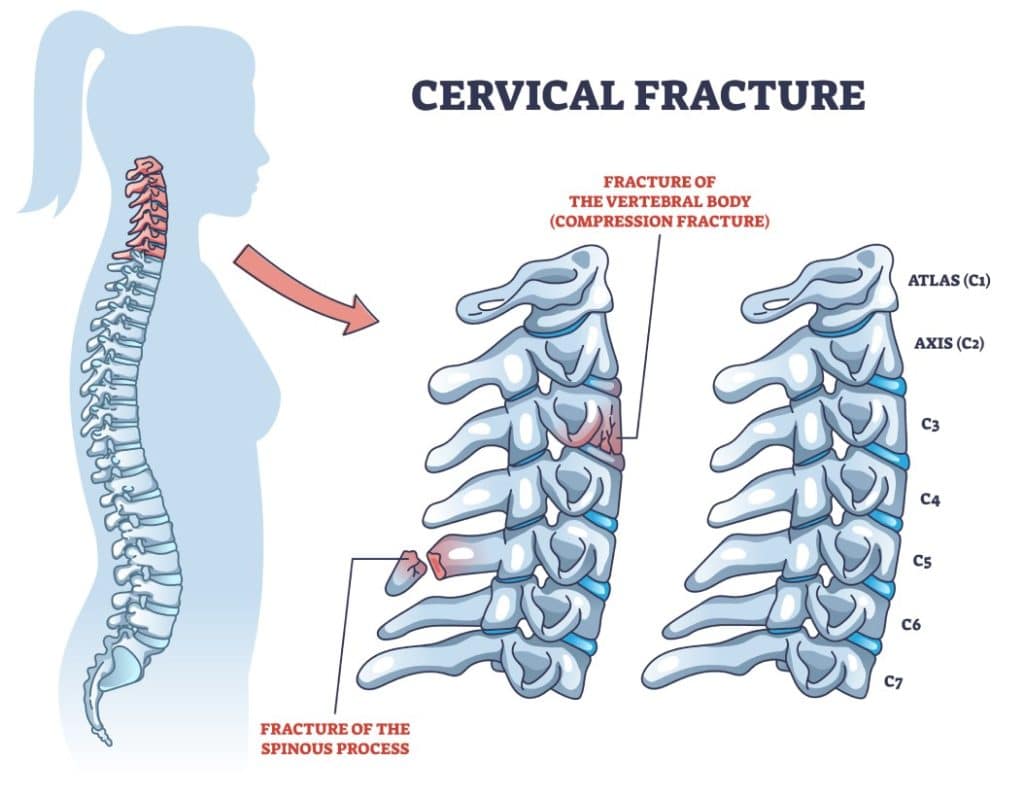
Any trauma to the spine can result in injury to the spinal cord. This may be related to spinal fractures or instability. Sometimes even without a fracture or instability of the spine, injury can still occur. If somebody already has narrowing of the spinal canal and compression of the spinal cord (often without any symptoms) due to disc herniation or degenerative disease, then they are more prone to injury after a fall or accident. Sometimes even minor trauma may cause deterioration.
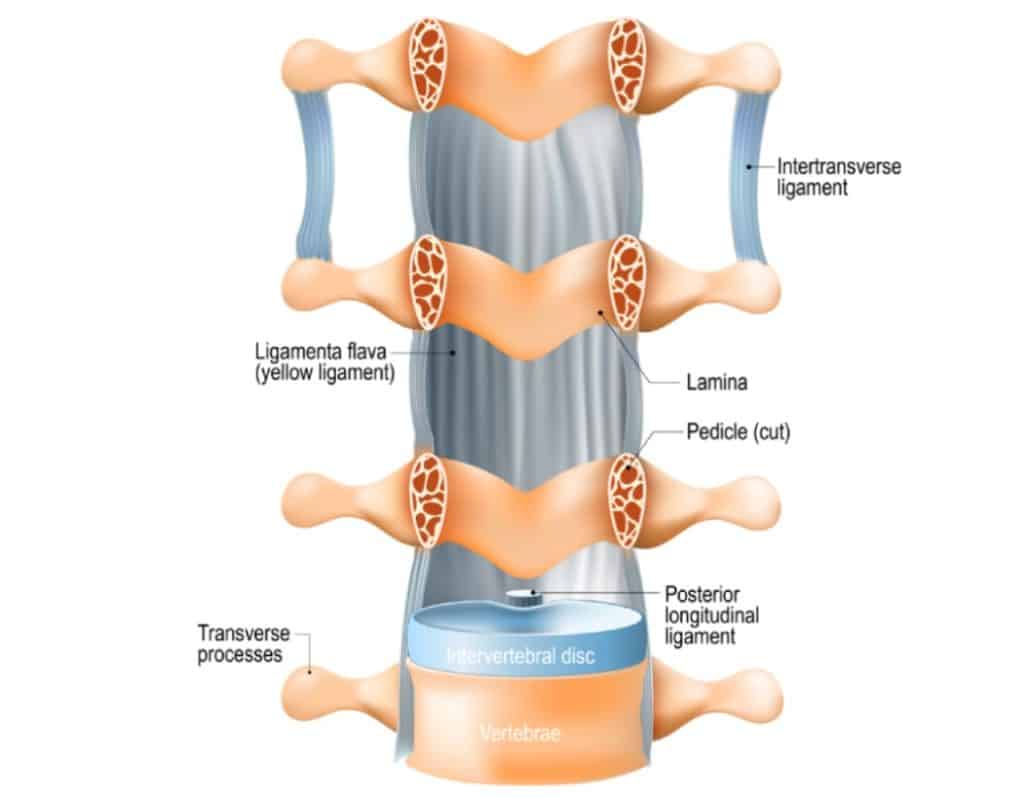
The cervical spine is more susceptible to ossification (or hardening) of the posterior longitudinal ligament (OPLL). This ligament runs along the posterior surface of the vertebrae and the discs inside the spinal canal. As the ligament hardens, it becomes thicker, less flexible and bone-like occupying more space inside the spinal canal, which can cause progressive spinal cord compression and cervical myelopathy.
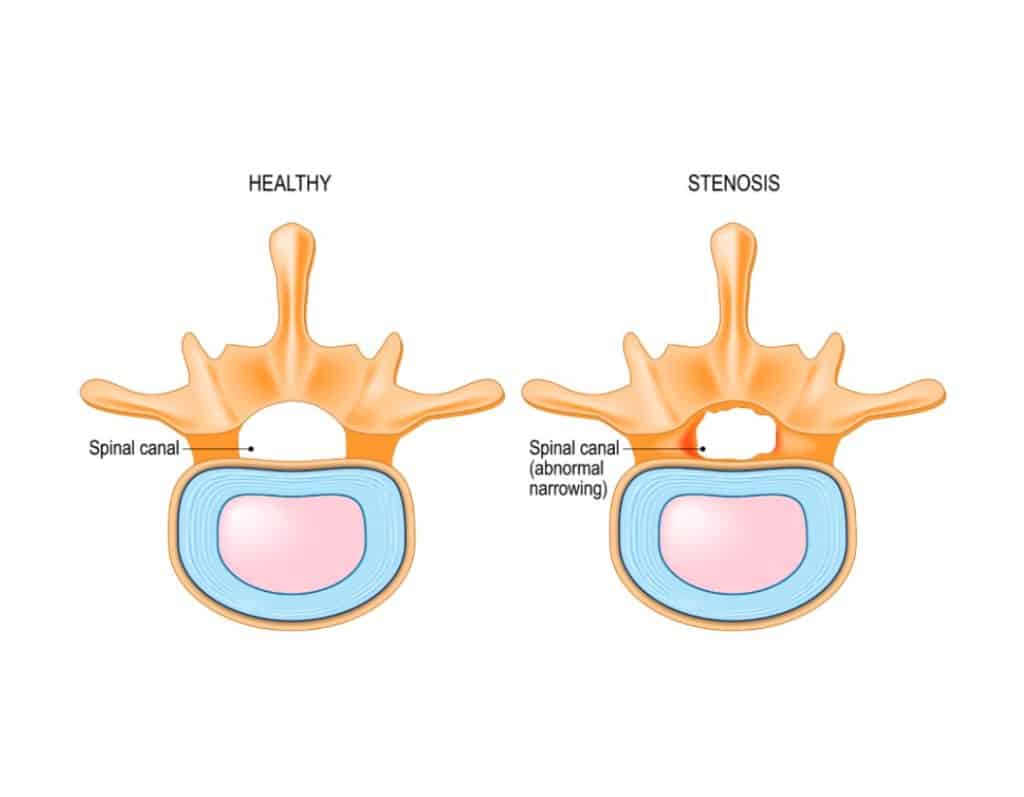
Some people are born with a narrow spinal canal (congenital narrowing) and may be more likely to have problems associated with cervical myelopathy at a younger age.
(cervical spinal stenosis with spinal cord compression)
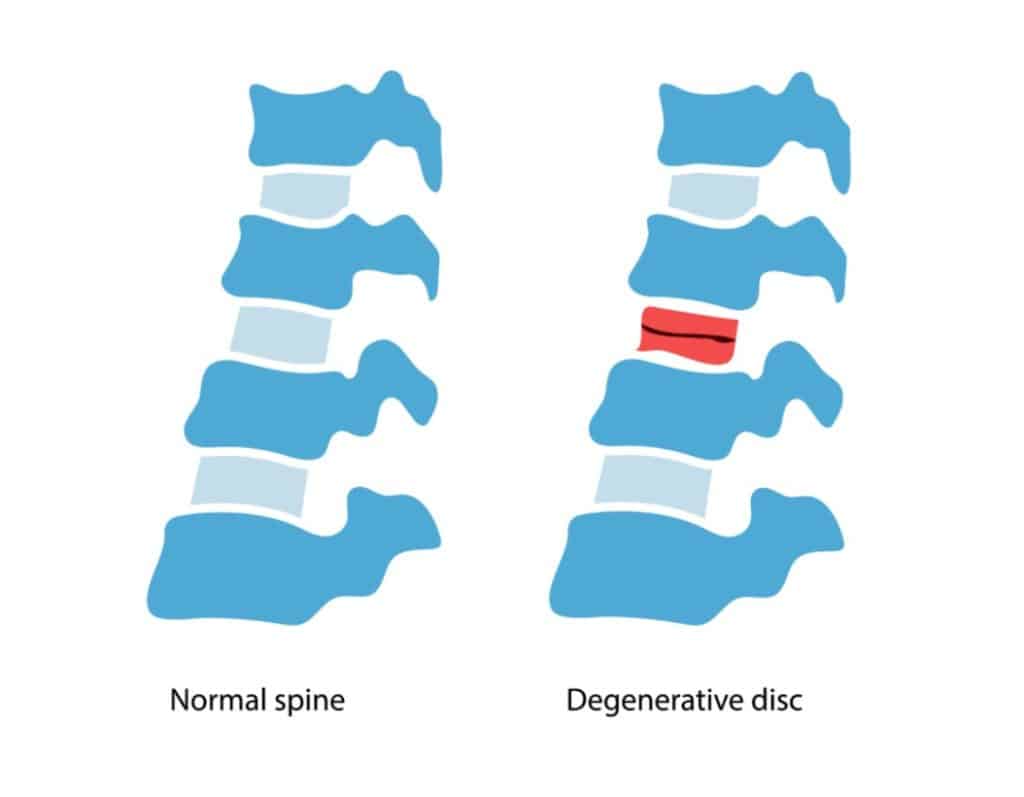
The discs, joints, bones and ligaments in our spine can degenerate as we get older, and bone spurs can form also. These degenerative changes can narrow the spinal canal where the spinal cord runs and cause compression of the spinal cord. These changes can also narrow the openings where the nerve roots exit the spine (exit foramina) and cause compression of the nerve roots. The symptoms and signs associated with this type of spinal cord compression is termed cervical spondylotic myelopathy. As this is an age-related phenomenon, cervical spondylotic myelopathy is more commonly found in those aged 50 and above.
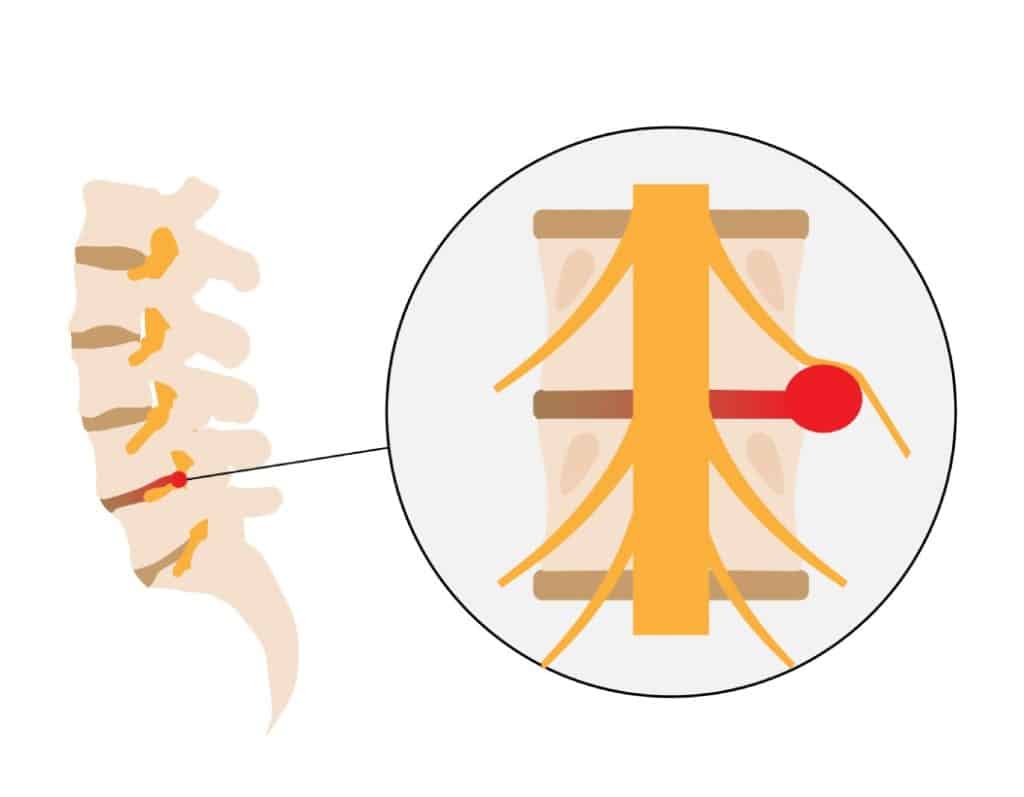
A herniated disc occurs when some of its centre contents leak out. The spinal disc is made up of a soft jelly-like content enclosed within a tough, rubbery shell. When a spinal disc herniates, its jelly-like content comes out, and it can compress and inflame the adjacent nerves. It can also cause compression of the spinal cord and result in cervical myelopathy. Physical activities, such as heavy lifting and extreme sports, can cause a herniated spinal disc.
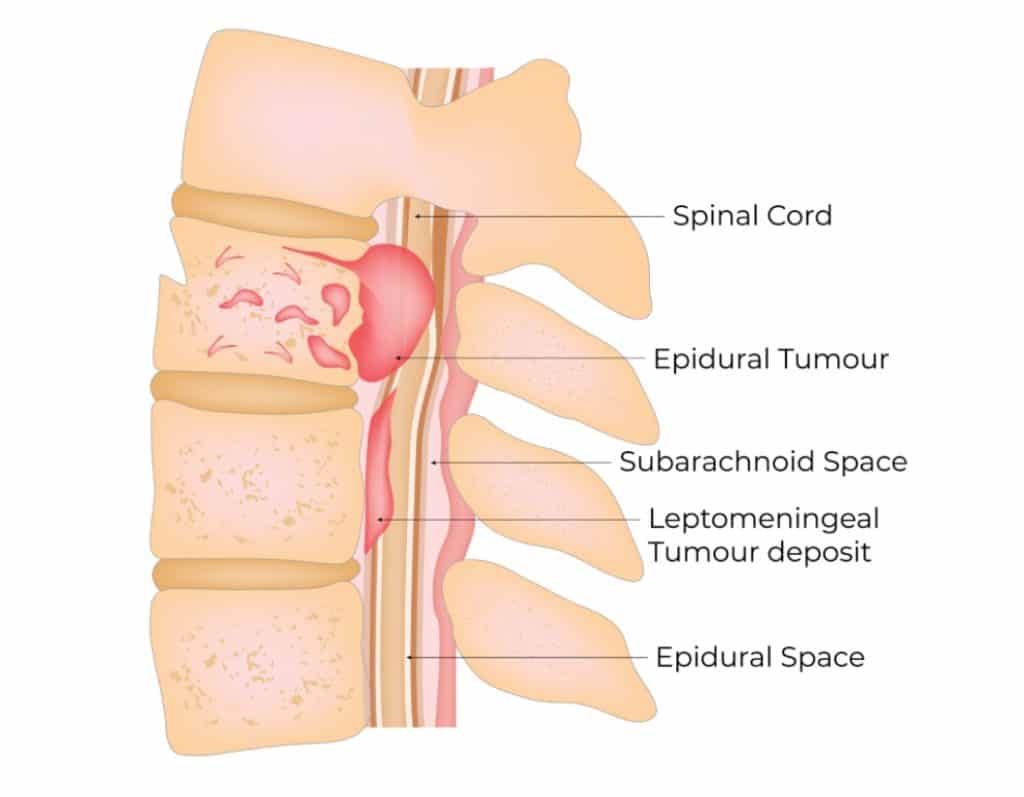
Less common causes of cervical myelopathy include spinal infection and spinal tumours. Certain inflammatory diseases, autoimmune conditions and other neurological disorders can also lead to myelopathy. These tend not to be due to compression of the spinal cord.
Neck pain and neck stiffness with reduced range of motion is a common symptom associated with degeneration in the cervical spine and is often present in patients with cervical myelopathy. The symptoms of cervical myelopathy are related to compression of the spinal cord. Patients with spinal cord compression often also have nerve root compression and may have symptoms related to both, including:
Degenerative changes in the cervical spine can compress either the spinal cord or the exiting nerve roots. Compression of the nerve roots produces a pattern of symptoms called cervical radiculopathy. It can occur on its own or alongside cervical myelopathy, so it is helpful to understand the distinction. Typical symptoms include:
The symptoms related to cervical myelopathy tend to get worse over time. Any deterioration in symptoms can be gradual or sudden (acute deterioration can occur with even minor trauma)

As spinal degeneration is a common cause of cervical myelopathy, age remains the biggest risk factor.
Lifestyle-related factors also affect your likelihood of developing cervical myelopathy. Maintaining an active, healthy lifestyle and avoiding smoking, and minimising alcohol consumption may reduce the chances of developing cervical myelopathy.
The symptoms of cervical myelopathy can overlap with a number of other conditions. Symptoms can often be dismissed as part of the ageing process. The diagnosis is usually made based on a clinical assessment by the cervical myelopathy specialist consisting of detailed history taking (focusing on things such as the onset of your problems and the change in your symptoms over time and whether there was any recent injury etc.) and physical examination findings. The clinical impression is usually confirmed on an MRI scan.
Non-surgical options can be considered and possibly effective for mild cases. This would involve medications for symptom relief and physical therapy.
If there is severe compression of your spinal cord and more severe symptoms, Dr Nolan, a spine doctor in Singapore may recommend surgical treatment to prevent further damage to the spinal cord and to allow for the possibility of recovery. These surgical treatments can be performed from the front or back of your neck, depending on the exact problem. The aim of surgery is to decompress the spinal cord (relieve pressure) and stabilise the spine when needed.
Lumbar spinal stenosis occurs when the space around the spinal nerves in the lower back becomes narrowed, leading to nerve compression. This can cause pain in the legs or lower back that worsens with walking and improves when sitting or leaning forward. Some people also experience numbness, tingling, burning or a sense of weakness. In severe cases, bowel or bladder control may be affected.
Lumbar spinal stenosis usually develops due to age-related changes such as disc degeneration, thickened ligaments, facet joint enlargement or herniated discs. Bone spurs or conditions like spondylolisthesis can also contribute. Risk increases with ageing, arthritis, previous spinal injuries, congenital narrowing, scoliosis, obesity and long-term poor posture. These factors do not directly cause stenosis but make degenerative narrowing more likely over time.
Treatment depends on symptom severity. Most people start with physiotherapy, anti-inflammatory medication, pain relief and mobility exercises. If symptoms persist, steroid injections or nerve blocks may help reduce inflammation. Surgery is considered when pain remains severe despite conservative care or when weakness or bowel or bladder issues occur. Procedures aim to relieve pressure on the nerves and may be performed using minimally invasive techniques.
Although lumbar spinal stenosis cannot be fully prevented, healthy habits can reduce its impact. Regular exercise helps maintain flexibility and strengthen the muscles that support the lower back. Low-impact activities such as walking, swimming or cycling are often recommended. Keeping a healthy weight reduces strain on the spine, while good posture and proper lifting techniques help protect the back during daily activities.
Yes, lumbar spinal stenosis can return after surgery. Although many patients experience long-lasting relief, surgery does not stop age-related changes in the spine. Degeneration of discs, ligaments or joints may lead to renewed narrowing at the same level or a nearby one. Conditions such as spondylolisthesis can also contribute. If symptoms recur, treatment often starts with physiotherapy, medication or injections, with further surgery considered only when necessary.
Dr Colum Nolan is a Senior Consultant Neurosurgeon with over 20 years of experience, specialising in minimally invasive spine (keyhole) surgery and other spine procedures.
A graduate of the Royal College of Surgeons in Ireland, Dr Nolan underwent neurosurgical training in Ireland and Australia, followed by a fellowship in complex spine surgery at Addenbrooke’s Hospital, Cambridge, as well as rotations at the Orthopaedic Spine Unit in Norfolk and Norwich Hospital.
Dr Colum is committed to delivering compassionate, patient-centred care, combining surgical precision with a genuine dedication to improving his patients’ quality of life.

Make an Enquiry or Request an Appointment
Our friendly team is here to serve you. For urgent enquiries and appointment requests, please call or WhatsApp us directly.