Cervical myelopathy is a degenerative condition that results from compression of the spinal cord in the neck. This compression could be a result of a traumatic impact or injury to the spine, degenerative disease, herniated discs or congenital narrowing of the spinal canal in the neck.
The cervical spine is made up of seven vertebrae (bones) along with accompanying intervertebral discs (‘cushions’ or ‘shock absorbers’) between the vertebrae. The joints between the bones are called facet joints and are lined with cartilage. Ligaments also connect the bones to each other. These structures allow the movement of the neck and control stability and flexibility.
Cervical myelopathy can occur due to several reasons, including:
The discs, joints, bones and ligaments in our spine can degenerate as we get older, and bone spurs can form also. These degenerative changes can narrow the spinal canal where the spinal cord runs and cause compression of the spinal cord. These changes can also narrow the openings where the nerve roots exit the spine (exit foramina) and cause compression of the nerve roots. The symptoms and signs associated with this type of spinal cord compression is termed cervical spondylotic myelopathy. As this is an age-related phenomenon, cervical spondylotic myelopathy is more commonly found in those aged 50 and above.
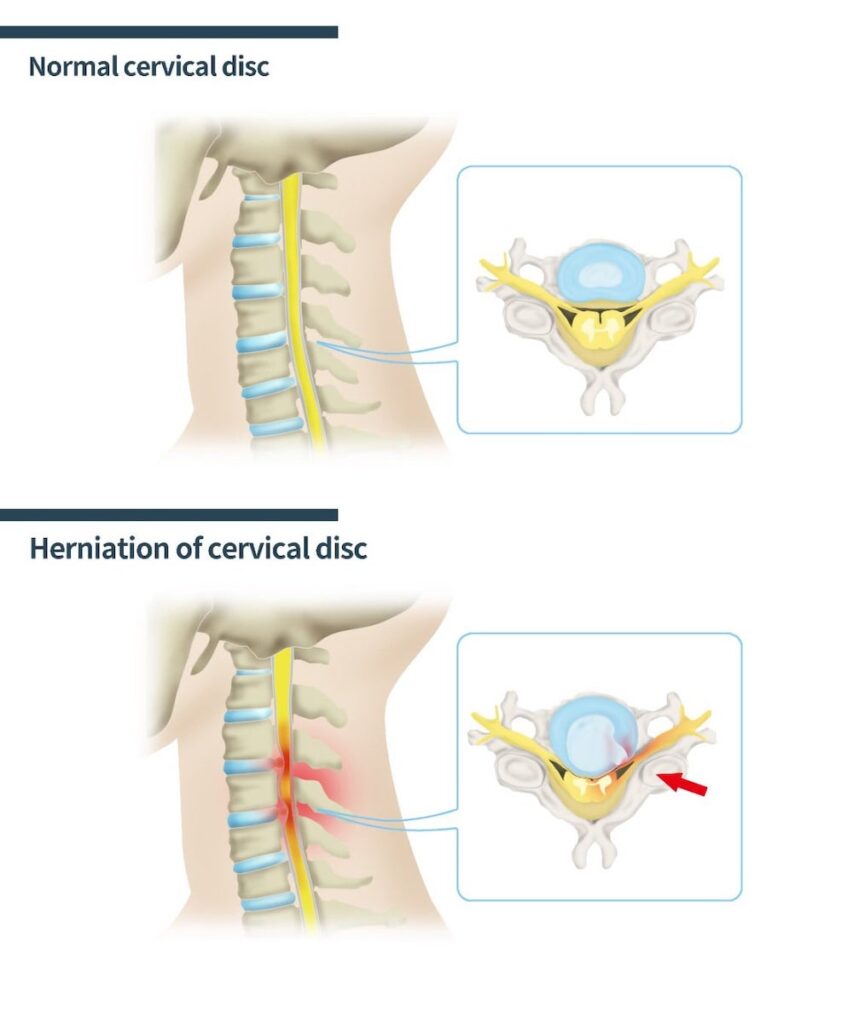
A herniated disc occurs when some of its centre contents leak out. The spinal disc is made up of a soft jelly-like content enclosed within a tough, rubbery shell. When a spinal disc herniates, its jelly-like content comes out, and it can compress and inflame the adjacent nerves. It can also cause compression of the spinal cord and result in cervical myelopathy. Physical activities, such as heavy lifting and extreme sports, can cause a herniated spinal disc.
Some people are born with a narrow spinal canal (congenital narrowing) and may be more likely to have problems associated with cervical myelopathy at a younger age.
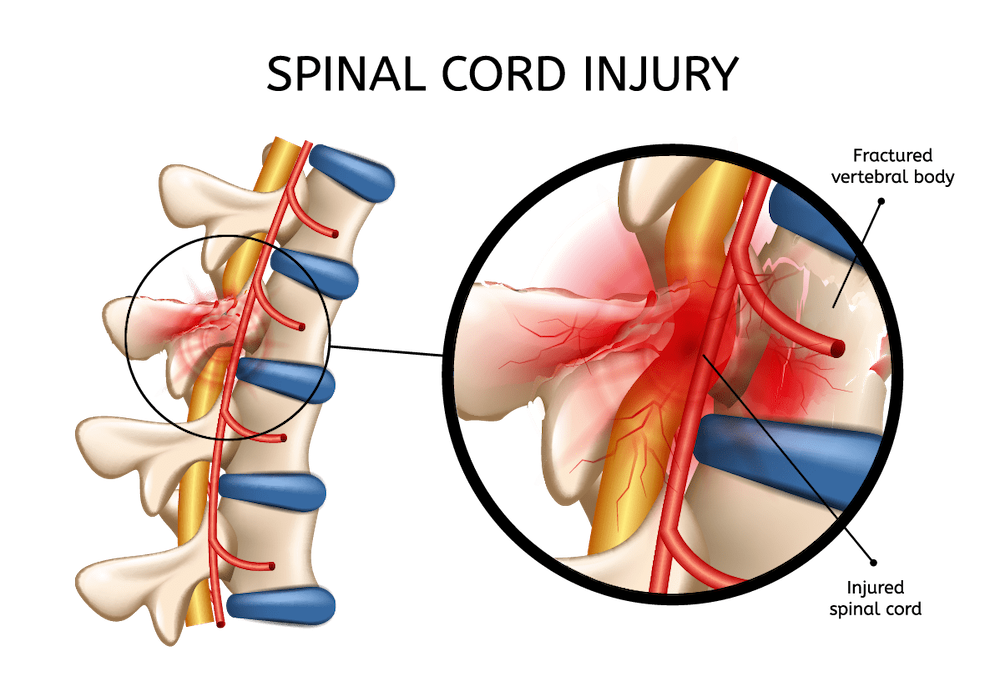
Any trauma to the spine can result in injury to the spinal cord. This may be related to fractures or instability of the spine. Sometimes even without a fracture or instability of the spine, injury can still occur. If somebody already has narrowing of the spinal canal and compression of the spinal cord (often without any symptoms) due to disc herniation or degenerative disease, then they are more prone to injury after a fall or accident. Sometimes even minor trauma may cause deterioration.
The cervical spine is more susceptible to ossification (or hardening) of the posterior longitudinal ligament (OPLL). This ligament runs along the posterior surface of the vertebrae and the discs inside the spinal canal. As the ligament hardens, it becomes thicker, less flexible and bone-like occupying more space inside the spinal canal, which can cause progressive spinal cord compression and cervical myelopathy.
Less common causes of cervical myelopathy include spinal infection and spinal tumours. Certain inflammatory diseases, autoimmune conditions and other neurological disorders can also lead to myelopathy. These tend not to be due to compression of the spinal cord.
Neck pain and neck stiffness with reduced range of motion is a common symptom associated with degeneration in the cervical spine and is often present in patients with cervical myelopathy. The symptoms of cervical myelopathy are related to compression of the spinal cord. Patients with spinal cord compression often also have nerve root compression and may have symptoms related to both. Symptoms are as follows:
The symptoms related to cervical myelopathy tend to get worse over time. Any deterioration in symptoms can be gradual or sudden (acute deterioration can occur with even minor trauma)
As spinal degeneration is a common cause of cervical myelopathy, age remains the biggest risk factor.
Lifestyle-related factors also affect your likelihood of developing cervical myelopathy. Maintaining an active, healthy lifestyle and avoiding smoking, and minimising alcohol consumption may reduce the chances of developing cervical myelopathy.
The symptoms of cervical myelopathy can overlap with a number of other conditions. Symptoms can often be dismissed as part of the ageing process. The diagnosis is usually made based on a clinical assessment by the cervical myelopathy specialist consisting of detailed history taking (focusing on things such as the onset of your problems and the change in your symptoms over time and whether there was any recent injury etc.) and physical examination findings. The clinical impression is usually confirmed on an MRI scan.
Non-surgical options can be considered and possibly effective for mild cases. This would involve medications for symptom relief and physical therapy.
If there is severe compression of your spinal cord and more severe symptoms of cervical myelopathy, Dr Nolan, a spine doctor in Singapore may recommend surgical treatment to prevent further damage to the spinal cord and to allow for the possibility of recovery. These surgical treatments can be performed from the front or back of your neck, depending on the exact problem. The aim of surgery is to decompress the spinal cord (relieve pressure) and stabilise the spine when needed.
Dr Colum Nolan clinical interests include degenerative and complex spinal disorders, cervical spine surgery, spinal tumours, spinal trauma, and endoscopy. He has particular expertise in minimally invasive spine surgery and the use of spinal navigation technology.
Prior to his private practice, he served as the Head of Service and Senior Consultant Neurosurgeon at the National Neuroscience Institute (NNI). He was also the Director of the Spine and Spinal Disorders Programme at NNI and was the head of Neurosurgery Service at Sengkang General Hospital.
No issue is too small.
Reach out to our friendly team.
No issue is too small.
Reach out to our friendly team.

No issue is too small.
Reach out to our friendly team.
No issue is too small.
Reach out to our friendly team.

No issue is too small.
Reach out to our friendly team.

No issue is too small.
Reach out to our friendly team.
© 2023 All Rights Reserved | Oxford Spine & Neuro | Terms & Conditions