
Dr Colum Nolan
Senior Consultant Spine & Neurosurgeon
MB, BCh, BAO, LRCPSI, MRCSI, FRCSI (Neurosurgery)
Is a term broadly used to refer to any manner of degeneration in the spine.
There are 33 individual bones (vertebrae) in the spine which are split up into 5 segments: 7 cervical vertebrae (neck), 12 thoracic vertebrae (upper back), 5 lumbar vertebrae (lower back), 5 sacral vertebrae and 4 vertebrae in the coccyx (tailbone).
In between each vertebra is a spinal disc that acts as a cushion or shock absorber and gives the spine its flexibility and stability. The joints between the bones (facet joints with cartilage) and the ligaments in the spine also provide flexibility and stability. The bones in the sacrum and coccyx are typically fused in adults. The cervical (neck) and lumbar (lower back) regions are the most mobile parts of the spine.
As we grow older, our bones, discs, joints/cartilage and ligaments that make up the neck and back develop age-related wear and tear. This natural wear and tear is referred to as cervical and lumbar spondylosis or degeneration of the cervical and lumbar spine. Signs of osteoarthritis may develop.
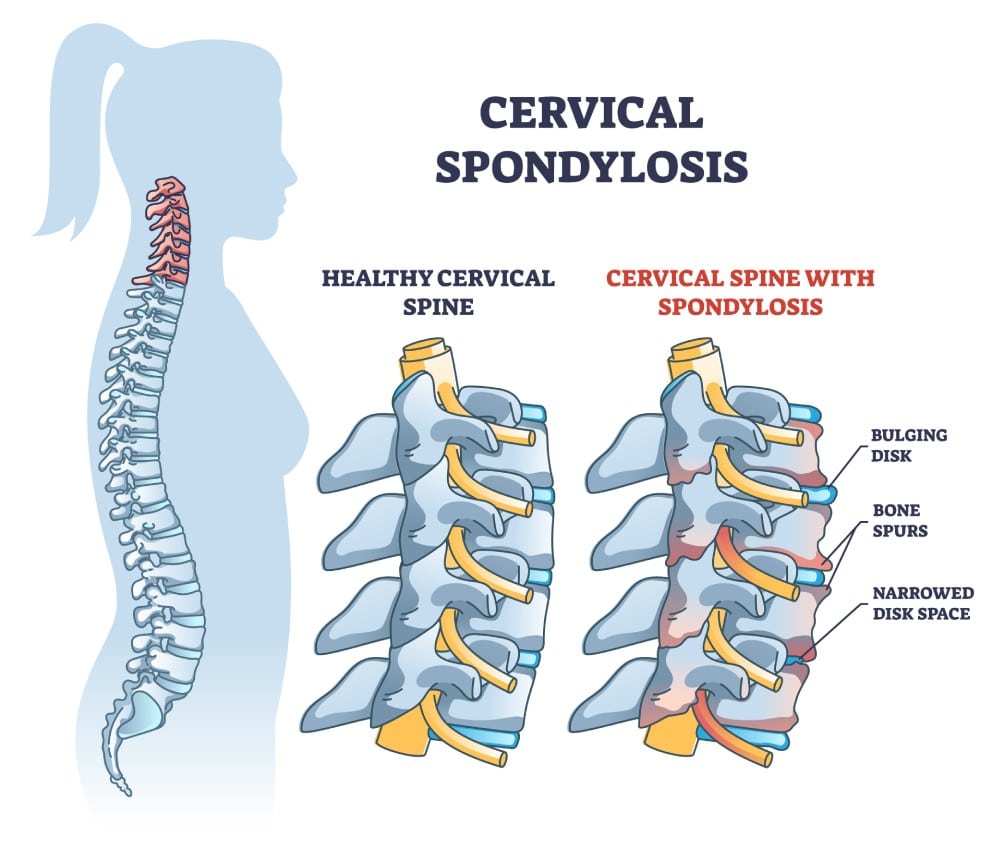
Spondylosis, especially cervical and lumbar spondylosis, is a condition that happens over time as part of the natural ageing process. Some changes that take place due to this ageing process include:

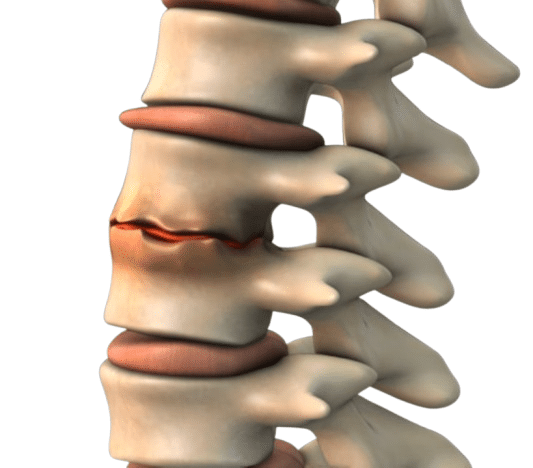
Most people’s spinal discs begin dehydrating and shrinking by the time they reach 40 years old. As your spinal discs start drying out, the cushion between each vertebra begins to thin, which allows more bone-on-bone contact between each vertebra.

Cracks (or fissures) can appear on the outer lining of your spinal discs leading to herniation that can sometimes compress and irritate the nerve roots in the spine or even the spinal cord. Disc herniations can also occur in younger people.
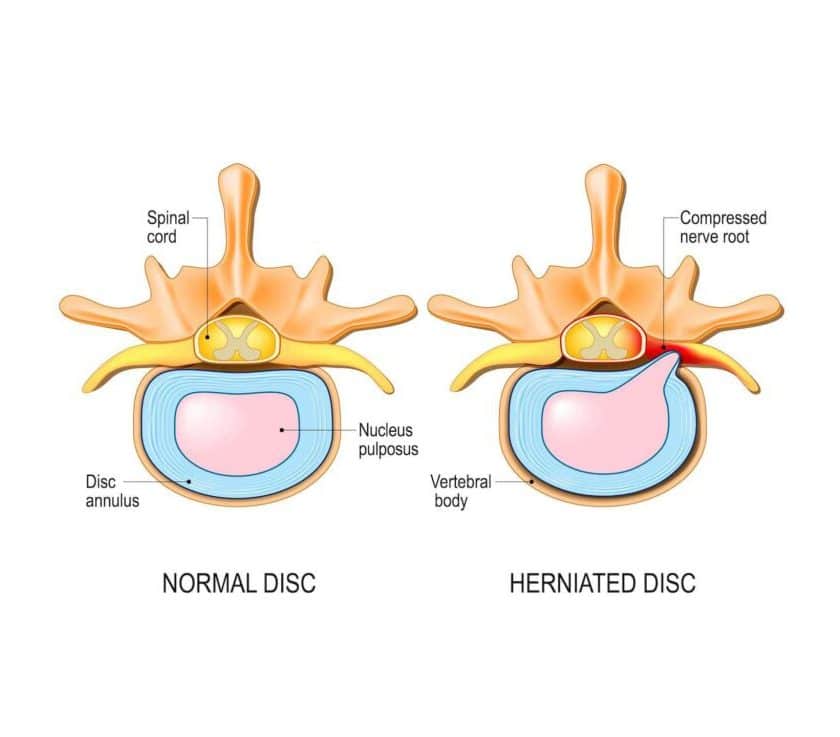
Degeneration of the spine often results in bone spurs that appear on the edge of the bones. This is the spine’s misguided effort in trying to strengthen itself by producing extra amounts of bone. These bone spurs can compress and irritate the nerve roots in the spine or even the spinal cord also.
Ligaments connect the vertebrae together, and as we age, these ligaments can start to stiffen – this is why we often tend to get ‘stiff necks’ or ‘stiff backs’ as we get older.

The joints between the bones in the spine can develop arthritis over time and cause neck pain or back pain.

Most people do not experience symptoms of spondylosis until later in life. When symptoms do occur, they tend to cause pain and stiffness in the neck or back. People can also experience muscle spasms or ‘popping’ or ‘grinding’ sensations when they move.
(Neck Pain and Stiffness)
Cervical spondylosis can lead to compression of the nerve roots in the neck region or compression of the spinal cord. This can cause additional symptoms such as:
Although rare, spinal infections can occur when a fungal or bacterial infection in another part of the body enters the spine through the bloodstream. Infected collections can irritate or compress nerve roots, causing cervical radiculopathy. TB infection can also occur in the spine.
Spinal tumours can also irritate and compress the nerve roots in the cervical spine resulting in symptoms suggestive of cervical radiculopathy.

(Neck Pain and Stiffness)
Lumbar spondylosis can lead to compression of nerve roots in the lower back. The spinal cord isn’t typically affected as it has already terminated in the upper lumbar region. Nerve root compression could lead to additional symptoms such as:

The greatest risk factor of cervical and lumbar spondylosis is ageing. Dehydrated and herniated discs, and bone spurs all develop as a result of ageing. In fact, over 85% of people aged 60 and above are affected by spondylosis but not everybody has symptoms.
Certain factors can put you at higher risk. For example, activities that put extra strain on your neck and back (i.e. bad/poor posture) can cause spondylosis. Any injury to the neck or back can also aggravate spondylosis.
Dr Colum Nolan is a Senior Consultant Neurosurgeon with over 20 years of experience, specialising in minimally invasive spine (keyhole) surgery and other spine procedures.
A graduate of the Royal College of Surgeons in Ireland, Dr Nolan underwent neurosurgical training in Ireland and Australia, followed by a fellowship in complex spine surgery at Addenbrooke’s Hospital, Cambridge, as well as rotations at the Orthopaedic Spine Unit in Norfolk and Norwich Hospital.
Dr Colum is committed to delivering compassionate, patient-centred care, combining surgical precision with a genuine dedication to improving his patients’ quality of life.

Make an Enquiry or Request an Appointment
Our friendly team is here to serve you. For urgent enquiries and appointment requests, please call or WhatsApp us directly.