Sciatica is one of the most common causes of lower back and leg pain, yet many people remain unsure what it truly means. In a recent episode of Every Body Knows, hosted by Mike Kasem and Catherine Robert, neurosurgeon Dr Colum Nolan, who specialises in spine conditions, shared clear and practical insights on how sciatica develops, what symptoms to look out for, and the steps involved in managing it.
The episode also featured radio personalities DJ Denise Tan (Gold 90.5FM) and DJ Sajini (Oli 96.8FM), who openly discussed their own experiences with sciatica and the challenges it brought to their daily lives.
This article draws from the key highlights of that discussion, offering an easy-to-read summary of the insights shared.
Watch the full episode here:
What Exactly Is Sciatica?
The sciatic nerve: where it runs
- It is the largest and longest nerve in the body
- Formed by nerve roots in the lower spine
- Travels through the buttock and down the back of the leg
- Branches into smaller nerves near the foot
When this nerve is compressed, pain can travel along its entire pathway — a hallmark feature of sciatica.
Recognising the Symptoms
- Sharp, shooting, or “electric-like” pain down the leg
- Pain that begins in the lower back or buttock
- Tingling, numbness, or burning sensations
- Difficulty sitting or standing for long periods
- Leg weakness in more severe cases
- Rare but urgent signs: changes in bowel or bladder control
What Causes Sciatica?
1. Slipped Disc (Disc Herniation)
A spinal disc acts as a cushion between vertebrae. When part of the disc’s inner gel pushes through its outer ring, it may press on the nerve roots that form the sciatic nerve. This is one of the most frequent causes of sciatica.2. Spinal Stenosis
As part of the natural aging process, the spine may undergo changes such as:- Disc thinning
- Bone spurs
- Thickened ligaments
Other contributing factors discussed include:
- Spondylolisthesis: one vertebra slipping forward over another
- Prolonged standing or repetitive heavy lifting
- Long periods of sitting or poor ergonomics
- Degenerative spine changes
- Diabetes, excess weight, and smoking
- Genetic predisposition
When Should You See a Spine Specialist?
- Persistent or recurring leg pain
- Numbness, tingling, or burning sensations
- Pain that affects daily function
- New or worsening leg weakness
- Bowel or bladder changes (urgent evaluation required)
How Sciatica Is Assessed
- A physical examination
- Understanding where the pain travels
- A trial of conservative treatment
- Disc herniation
- Nerve compression
- Spinal stenosis
- Degenerative changes
- Structural conditions such as spondylolisthesis
How Sciatica Is Treated: Step-by-Step
1. Conservative Treatment
Common first-line treatments include:- Medication for pain and inflammation
- Physiotherapy to improve mobility, posture and core strength
- Heat or cold therapy
- Activity modification
- Ergonomic adjustments at work
- Supportive options such as acupuncture or TCM
2. Minimally Invasive Spine Surgery (When Indicated)
For individuals with persistent symptoms or significant nerve compression, minimally invasive spine surgery may be considered. These modern techniques involve small keyhole incisions, allowing the surgeon to decompress the affected nerve with:- Minimal tissue disruption
- Lower complication risk
- Faster recovery
- Earlier return to activity
Tips to Reduce the Risk of Sciatica
Dr Colum also shared several practical prevention tips:
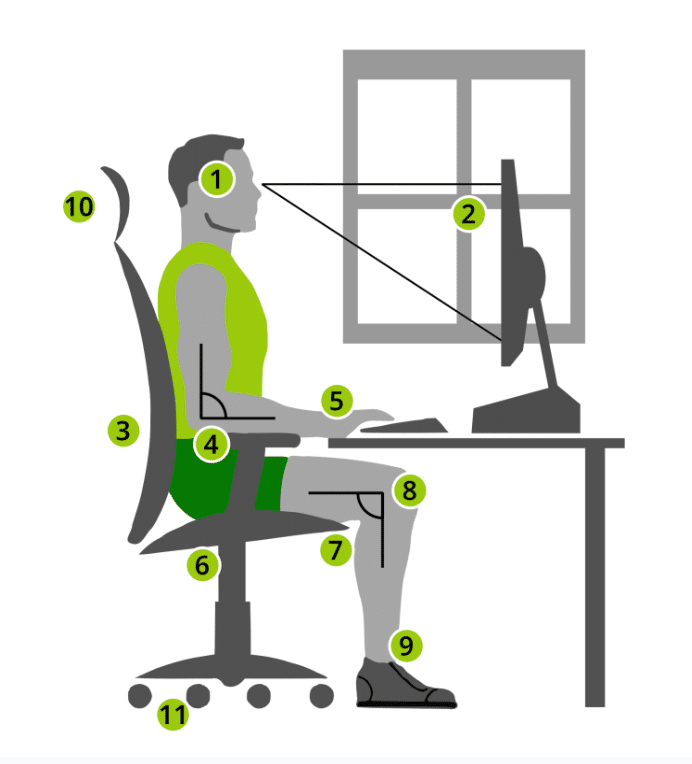
- Maintain good posture while sitting and standing
- Use safe lifting techniques
- Keep a healthy weight
- Stay active within comfortable limits
- Manage conditions such as diabetes
- Avoid smoking
- Optimise desk ergonomics or use a standing desk
- Strengthen the back and core with guidance
These habits support long-term spinal health and may help reduce the recurrence of symptoms.
Key Takeaway
Sciatica can significantly affect daily life, but many people improve with timely assessment and conservative care.
Understanding the underlying cause — whether a slipped disc, spinal stenosis, or structural change — helps guide appropriate treatment.
If symptoms persist, interfere with movement, or are accompanied by weakness, consulting a spine specialist, spine surgeon, or neurosurgeon specialising in spine can help ensure that the right steps are taken early.

