Have you ever had a sharp, burning, or throbbing pain in your neck? Did you also experience weakness, numbness and tingling sensation alongside the pain? If yes, these symptoms may have been caused by a pinched nerve in the cervical (neck) part of your spinal column, also known as your spine, backbone or vertebral column.
Your spine consists of thirty-three bones, starting at your neck and ending at the tailbone. Each bone has a spinal canal that protects the spinal cord, which carries nerves that send and receive signals. Between these bones are intervertebral discs that cushion and protect the spine. Conditions like spinal stenosis, bone spurs, or herniated discs can compress spinal nerves, leading to pain, numbness, and weakness. A herniated disc occurs when the soft inner part of the disc slips through a tear in the outer layer, commonly affecting the lumbar and cervical vertebrae. The C5-C6 and C6-C7 vertebrae are typical sites of disc herniation, and treatments like Anterior Cervical Discectomy and Fusion or Artificial Disc Replacement may be recommended for compressed nerves.

Anterior Cervical Discectomy and Artificial Disc Replacement or Fusion is a surgical procedure done to relieve pressure on a compressed nerve, alleviate symptoms and restore any lost function or sensation.
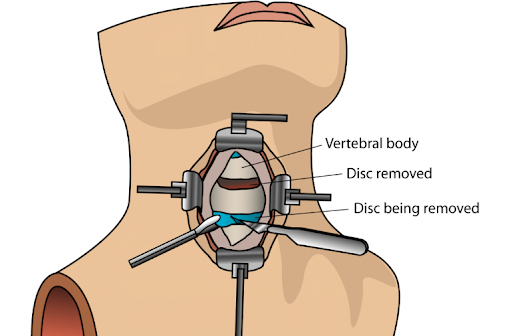
In an Anterior Cervical Discectomy and Artificial Disc Replacement or Fusion surgery, your Spine surgeon makes incisions through the front of your neck or throat and removes the affected disc causing the compression effect. The cervical vertebral bones or bodies are then fused together, or an artificial disc may be introduced to replace the affected disc that was removed.
This procedure is considered a major surgery, and it is made up of two parts:

An Anterior Cervical Discectomy and Artificial Disc Replacement or Fusion is done to relieve symptoms of a compressed spinal nerve which could be caused by arthritis or age-related degenerative bone spurs, herniated disc or spinal stenosis. Conditions that should be satisfied to determine if you need an anterior cervical discectomy and artificial disc replacement or fusion include:
At Oxford Spine and Neurosurgery Centre, a specialist clinic in Singapore, our experienced neurosurgeon will thoroughly assess your suitability for Anterior Cervical Discectomy and Artificial Disc Replacement.
An anterior cervical discectomy and artificial disc replacement or fusion can offer significant benefits, which include the following:

During your visit to Oxford Spine and Neurosurgery Centre, you may undergo the following:
On your appointment date, you will be taken to the operating room, where anaesthesia, which may be local or general, will be administered. Your vital signs, such as your respiratory rate, blood pressure, and heart rate, will be monitored.
During an anterior cervical discectomy and artificial disc replacement or fusion, your spine surgeon makes small 1 to 2-inch horizontal incisions to the left or right of your neck. These horizontal inches usually follow the natural neck creases. The structures such as fascia, muscles, trachea and oesophagus are retracted to reveal the affected disc. The exact cervical vertebrae are visualised using a particular type of x-ray. The disc is then completely removed.
After the disc has been removed, the affected vertebrae are joined or fused. A bone graft will be placed in the space formerly occupied by the intervertebral disc, or an artificial disc may replace it.
After your neck surgery, you will be moved from the operating theatre to a recovery ward for a day or two for further monitoring of your vital signs and any complications. You will also be given medications to relieve any pain experienced. Your surgeon will provide specific advice on when you can resume normal activities.
You may need to wear a cervical collar or a neck brace to limit excessive neck movement. Your spine surgeon may also ask you to commence physical therapy.
Anterior Cervical Discectomy and Artificial Disc Replacement or Fusion has a high success rate. According to a 10-year prospective study of patients who underwent anterior cervical discectomy and artificial disc replacement or fusion, a success rate of 85% to 95% success was reported by the patients.
ACD Success Rates:
Artificial Disc Replacement (ADR) Success Rates:
These statistics highlight the effectiveness of both procedures, with consistent patient-reported success and clinical outcomes. However, patient health status, surgeon expertise, and postoperative care significantly determine long-term success.
As with any other surgery, there are risks involved. Some of the common risks associated with this form of spine surgery include:
Recovery time for an anterior cervical discectomy and artificial disc replacement or fusion varies from person to person, depending on the individual’s health status, the complexity of the surgery, the presence of complications, and adherence to procedure instructions.
The immediate recovery time is usually several weeks. During this period, you may experience some pain and discomfort, so it is important to follow your doctor’s instructions regarding neck movement, stopping strenuous movements, physical therapy, and adherence to your pain relief medications. You may also wear a neck brace during this period.
A few months after the procedure, your symptoms should have reduced significantly, and you should be able to fully return to your usual regular activities, except for very strenuous activities. The joined vertebrae may take up to 12 months to fuse fully. Regular attendance at your clinic appointment is important to monitor and enhance recovery.
For personalised guidance on your suitability for Anterior Cervical Discectomy and Artificial Disc Replacement or Fusion, book an appointment with Oxford Spine and Neurosurgery Centre to consult Dr Colum Nolan, Senior Consultant Neurosurgeon.
Dr Colum Nolan is the Medical Director at Oxford Spine and Neurosurgery Centre, Mount Elizabeth Novena Hospital in Singapore. He is an experienced Senior Consultant Neurosurgeon with a subspecialty in Spine Surgery.
With over 15 years of experience, Dr Colum’s clinical interests include degenerative and complex spinal disorders, cervical spine surgery, spinal tumours, spinal trauma, and endoscopy. He has particular expertise in minimally invasive spine surgery and spinal navigation technology for enhanced accuracy and safer surgery, and he uses techniques such as artificial cervical disc replacement as an alternative to spinal fusion.
